|
Tackle hepatitis C to save people living with HIV

By Shobha Shukla, CNS
June 18, 2014
The author is the Managing Editor of Citizen News Service - CNS. She is a J2J Fellow of National Press Foundation (NPF) USA and received her editing training in Singapore. She has earlier worked with State Planning Institute, UP and taught physics at India's prestigious Loreto Convent. She also co-authored and edited publications on gender justice, childhood TB, childhood pneumonia, Hepatitis C Virus and HIV, and MDR-TB. Email: shobha@citizen-news.org, website: www.citizen-news.org
The WHO recognizes that the ‘silent epidemic’ of viral hepatitis affects a large part of the world’s population causing over 1.4 million deaths every year, yet remains largely unknown or ignored. It is estimated that 240 million people are chronically infected with hepatitis B virus (HBV) and more than 185 million people are infected with the hepatitis C virus (HCV). These numbers far exceed the number of people living with HIV (PLHIV) estimated at 34 million.
Viral hepatitis co-infection in PLHIV is now recognized as a major public health problem resulting in increased morbidity and mortality among PLHIV including those on antiretroviral therapy (ART). Chronic HBV infection affects 10% of PLHIV worldwide. Chronic HCV infection affects 20% of PLHIV, with a majority of them living in low- and middle-income countries. In countries where injecting drug use is the biggest risk factor for HIV transmission, as many as 7 out of 10 PLHIV are co infected with HCV. In countries where sexual behavior is the biggest risk factor for HIV transmission, HCV co infection is less common, but still a concern, with about 1 in 10 PLHIV being co infected with HCV.
HCV is a blood borne virus, most commonly transmitted through contact with the blood of an HCV-infected person, through sharing contaminated needles/drug use equipment and blood transfusion. Less commonly, it is transmitted through sexual contact with an HCV-infected person, or through birth to an HCV-infected mother. HCV is a much smaller virus than HIV, so there is a lot of it even in a tiny amount of blood, but unlike HIV, HCV can stay alive on surfaces outside the body for many days. HCV is 10 times more infectious than HIV.
Experts agree that co infection with HCV makes HIV treatment more complicated. A liver damaged from HCV may cause HIV medications to become less effective and more toxic. HCV co infection triples the risk for liver toxicity from HIV medicines. Also, HIV- HCV co infection more than triples the risk for liver disease and liver-related death from HCV.
HCV has 6 different variants - genotypes 1, 2, 3, 4, 5, and 6 with further subdivisions in each genotype. This variability has made it difficult to develop a vaccine that will protect against all HCV strains. However, unlike HIV infection, Hepatitis C can be cured by treatment. WHO recommends pegylated and standard interferon (PEG-IFN) in combination with ribavirin (RBV) to be used for the treatment of chronic HCV infection.
Persons infected with genotypes 1 and 4 are treated with PEG-IFN/RBV for 48–72 weeks, while those infected with genotypes 2 and 3 are treated with PEG-IFN/RBV for 24–48 weeks. The longer treatment durations are recommended for persons co infected with HIV and those with advanced fibrosis or cirrhosis. Persons with genotype 1 infection and an extended rapid virological response are treated with a shortened course of 24 weeks of PEG-IFN/RBV.
Dr Franco Buonaguro, Director, Unit of Molecular Biology and Viral Oncology, Napoli, Italy, told Citizen News Service (CNS) that, “The treatment response of HCV for pegylated interferon and ribavirin is 46% in patients with Genotype 1 and 76% in patients with genotypes 2 and 3, which in case of PLHIV co-infected with HCV reduces drastically to 20% for genotype 1 and 62 % for type 2 and 3.”
Thus not only duration of treatment for HCV in PLHIV is longer, but treatment response is also poorer. Coupled with this is the high cost of treatment (US$ 2 000 in Egypt for 48-weeks of PEG/IFN RBV), and the high rate of adverse events which require regular monitoring, which prevents most patients from receiving treatment in most low- and middle-income countries.
The field of HCV therapeutics is however evolving rapidly. New oral drugs sofosbuvir (a specific HCV polymerase inhibitor approved by the FDA in December 2013 ) and simeprevir, known as direct-acting antivirals (DAAs) have the potential to revolutionize treatment, with expected cure rates higher than 90% for some genotypes of the disease. The new guidelines of WHO strongly recommend treatment using sofosbuvir and RBV for genotypes 1, 2, 3 or 4 of the disease, with or without PEG-IFN, depending on the genotype.
Dr Buonaguro said that, “Sofosbuvir treatment regimens and duration are dependent on both viral genotype and patient population. Patients with genotype 1 or 4 are treated with sofosbuvir plus PEG-IFN and RBV for 12 weeks; those with genotype 2 or 3 are part of an all oral drug regimen of sofosbuvir plus RBV for 12 or 24 weeks respectively. The PHOTON-1 study evaluated sofosbuvir and RBV for 12 weeks in patients with genotype 2 HCV infection co-infected with HIV-1 and for 24 weeks in patients with genotypes 1 or 3 HCV co-infected with HIV-1. Trial participants achieved treatment cure rates of 76-92%.”
But the only deterrent is the prohibitively high price of the DAAs with a 12 weeks Sofosbuvir treatment costing US $84,000 in the US. At these prices, access in low and middle-income countries is likely to be extremely limited. Moreover the new medicines have yet to be licensed in most countries.
Generic production of drugs for HCV can reduce the cost drastically, as had happened in the case of anti retrovirals for HIV. A study done at Liverpool University shows that a 12-week course of sofosbuvir could cost as low as $68-$136. But a word of caution here from Dr Gourdas Choudhuri, Director and Head of Department of Gastroenterology and Hepatobiliary Sciences at Fortis Healthcare, India: “While generics are well established for chemical compounds, where efficacy can be tested, HCV drugs have to be tested in terms of bio efficacy too, and not just by way of chemical structures. So there will need to be a little more reassurance from companies launching generic interferons about their effectiveness.”
Nonetheless all PLHIV should be tested for HCV. A new global resolution endorsed by all 194 member states at the 67th session of WHA in May 2014, has called for enhanced action to improve equitable access to viral hepatitis prevention, diagnosis, and treatment and requested the WHO Secretariat to facilitate access to affordable treatment.
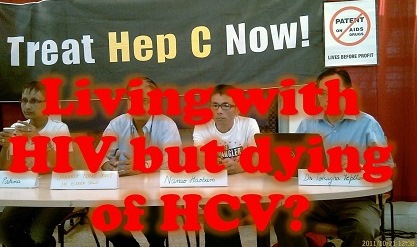
During a CNS press conference at the 19th International AIDS Conference in 2012, Eldred Tellis, Director of the Sankalp Rehabilitation Trust, Mumbai, India, had rightly said that, "It makes public health sense to link HCV prevention efforts to HIV programmes. Prevention and harm reduction efforts for HIV and HCV with vulnerable communities should go hand in hand. Unless this is done, HCV infections will rise even though HIV transmission rates reduce, particularly among injecting drug users – the most vulnerable community."
The HIV Programme is committed to increase its focus on viral hepatitis and HIV co-infection in 2014–2015. Let us hope that the forthcoming XX International AIDS Conference (AIDS 2014) in Melbourne will provide renewed impetuous to making timely viral hepatitis diagnosis and treatment affordable and accessible to all those in need of it.
--- Shared under Creative Commons (CC) Attribution License
Posted on: June 25, 2014 04:42 PM IST
|